Publications
Teratology Primer, 3rd Edition
Does Obesity Increase the Risk of Having a Child with a Birth Defect?
Sarah C. Tinker and Janet D. Cragan, National Center on Birth Defects and Devlopmental Disabilities, Centers for Disease Control and Prevention, Atlanta GA
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The prevalence of obesity in the United States has more than doubled in the past 50 years, and currently approximately one-third of women of childbearing age have obesity. One concern about the high prevalence of obesity, defined as body mass index greater than 30 kg/m2, among this population is the consistently observed association between maternal prepregnancy obesity and an increased risk for certain birth defects.
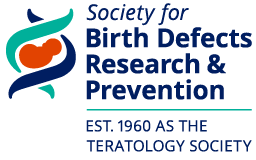
Neural tube defects (NTDs) are the birth defects most consistently associated with maternal prepregnancy obesity. A 2009 meta-analysis estimated that the risk for NTDs was almost twice as high among obese women relative to women with a normal BMI (18.5 – 24.9 kg/m2), based on data from nine different studies (Figure 1). Data published subsequently have been consistent with these results. When specific NTDs have been assessed, a slightly stronger association is observed for spina bifida relative to anencephaly (Figure 1).
Prepregnancy obesity is associated with a modestly increased risk for congenital heart defects (CHDs), when considered as a group (Figure 1). Associations with prepregnancy obesity have been observed for certain broad categories of CHDs, including septal defects, conotruncal defects, and left and right ventricular outflow tract obstruction defects; associations with specific defects include hypoplastic left heart syndrome, atrial septal defects, Tetralogy of Fallot, transposition of the great arteries, coarctation of the aorta, and pulmonary valve stenosis. However, results across studies show considerable heterogeneity.
Relatively consistent, but modest, associations with obesity have been observed for orofacial clefts (Figure 1). It appears that these associations may be limited to cleft palate with or without cleft lip (Figure 1). Other defects that have been studied less thoroughly, but for which associations with prepregnancy obesity have been observed, include hydrocephaly, limb reduction defects, and anorectal atresia. In contrast, gastroschisis is strongly inversely associated with prepregnancy obesity; being underweight prior to pregnancy is associated with an increased risk for gastroschisis. The reasons for the opposite pattern of association for this defect relative to others is unknown.
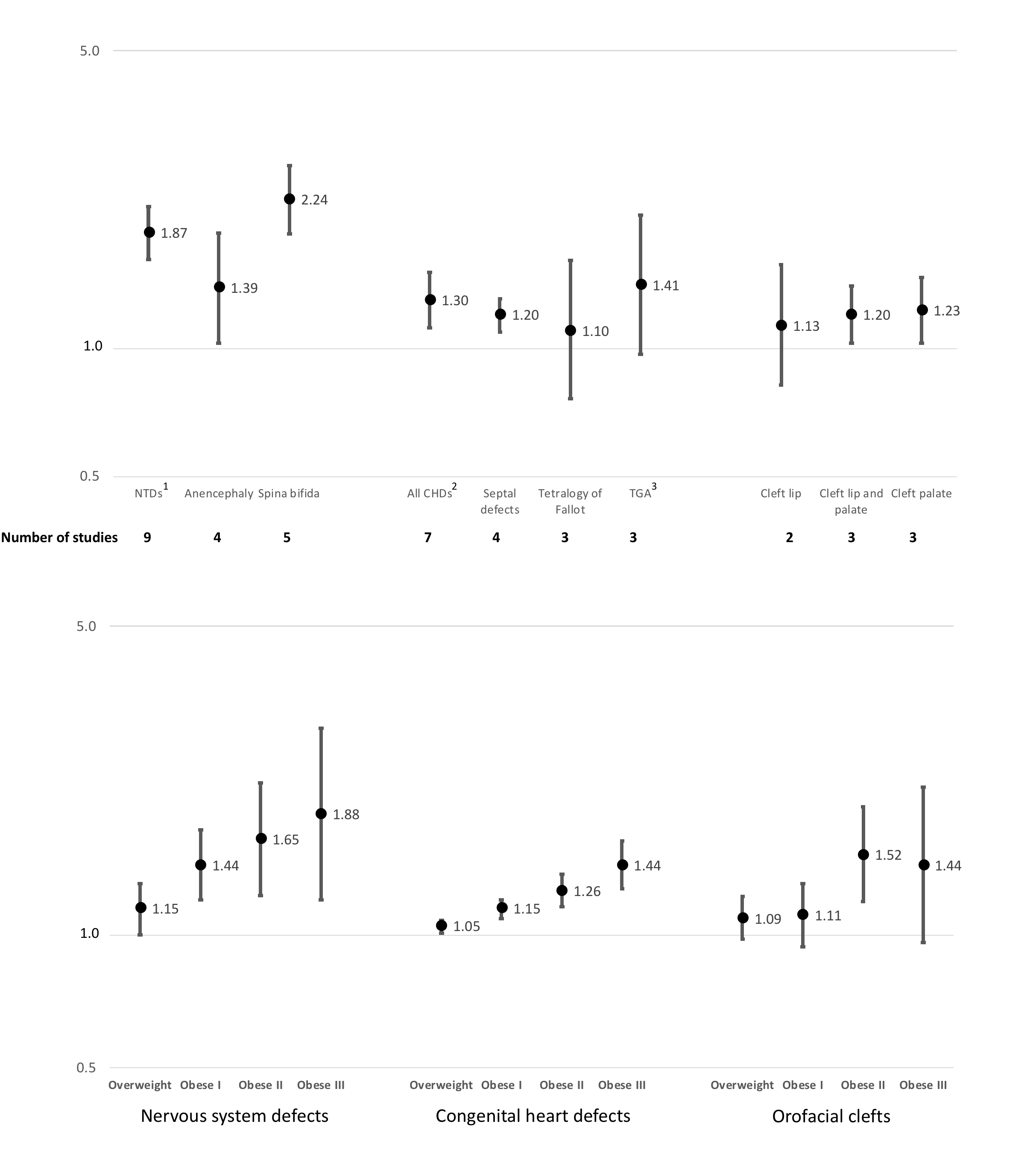
Associations between being overweight (BMI 25.0 to 29.9 kg/m2) and birth defects tend to be more modest (e.g., NTDs) or absent (e.g., cleft palate) compared with birth defects associated with obesity. In studies that were able to assess different degrees of obesity, the association with certain defects became stronger with increasing obesity. In a 2008 meta-analysis, a dose-response was observed for summary odds ratios. The risk of NTDs among overweight, moderately obese, and severely obese women compared to normal weight women was 1.2, 1.7, and 3.1 times higher, respectively. Results from a meta-analysis focused on CHDs also demonstrated a dose-response with obesity levels for all CHDs combined; the pooled odds ratios were 1.1, 1.2, and 1.4 for overweight, moderately obese, and severely obese, respectively. When specific CHD categories were examined, the risk for pulmonary valve stenosis and atrial septal defects showed a dose-response with levels of obesity. Data from a large population-based cohort study of over 1.2 million singleton births in Sweden showed a dose-response for increasing BMI category and increasing risk for several birth defects classified by broad categories, including nervous system defects, CHDs, orofacial clefts, digestive system defects, genital organ defects, and limb defects (Figure 2). Sub-categories of obesity were defined differently across studies, with the cut-point between moderate and severe obesity ranging from 35 to 40 kg/m3 or defined by a maximum weight (>240 to >260 lbs).
The mechanism through which obesity affects the risk for birth defects is not well understood. If causal, a likely pathway is through metabolic dysfunction. Pregnant women with uncontrolled diabetes have an increased risk for certain birth defects, including NTDs. When pregnant women with diabetes maintain tight glycemic control, however, their risk for birth defects decreases to match that of the general population, implicating hyperglycemia as a potential mechanism. Obesity increases the risk for non-insulin dependent diabetes and hyperglycemia. While the majority of studies of obesity and birth defects exclude women with pregestational diabetes, women with undiagnosed diabetes would be included in these studies. It is also possible that hyperglycemia at levels below the diagnostic threshold for diabetes have a negative impact on fetal development.
Prenatal diagnosis of birth defects is more challenging in women who are obese. Women with obesity may therefore have a lower rate of prenatal diagnosis of birth defects and fewer pregnancy terminations, which would result in a higher birth prevalence of defects and biased results from studies that ascertain only live births. Obesity also increases the risk for infertility, and use of fertility treatments has been associated with an increased risk for certain birth defects. Other possible non-causal explanations for the observed association between obesity and the risk for certain birth defects include nutritional issues, such as poor diet quality or lower folic acid intake, and sociodemographic factors.
The American College of Obstetricians and Gynecologists recommends that women achieve a healthy weight prior to pregnancy. However, effective treatments for obesity are limited and the safety of their use immediately before conception is unknown. Furthermore, almost half of U.S. pregnancies are unplanned, and weight loss during pregnancy is not recommended. Future research could help toward understanding the mechanisms through which obesity is associated with the risk for certain birth defects in order to develop effective interventions and prevention measures.
Suggested Reading
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No 156: Obesity in Pregnancy. Obstet Gynecol 2015;126(6): 112-126.
Cai GJ, Sun XX, Zhang L, Hong Q. Association between maternal body mass index and congenital heart defects in offspring: a systematic review. Am J Obstet Gynecol 2014;211(2):91-117.
Correa A, Marcinkevage J. Prepregnancy obesity and the risk of birth defects: an update. Nutr Rev 2013;71 Suppl 1:S68-77.
Persson M, Cnattingius S, Villamor E, et al. Risk of major congenital malformations in relation to maternal overweight and obesity severity: cohort study of 1.2 million singletons. BMJ 2017;357:j2563.
Rasmussen SA, Chu SY, Kim SY, et al. Maternal obesity and risk of neural tube defects: a metaanalysis. Am J Obstet Gynecol 2008;198(6):611-619.
Stothard KJ, Tennant PW, Bell R, and Rankin J. Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis. JAMA 2009;301(6):636-650.
Information about specific types of birth defects: https://www.cdc.gov/ncbddd/birthdefects/types.html